
Photo courtesy of Lukasz Szmigiel on unsplash.com
For most folks, when you reach age 65 and have ceased regular work, filing for Medicare Parts A & B is an automatic thing. If you don’t file during the 3 months before or after your 65th birthday, you may have penalties to pay. This applies even if you have recently been laid off of work and are covered for health insurance under a COBRA plan. Part A carries no cost if you’re fully covered (40 quarters of coverage), but Part B requires a monthly premium.
When laid off from an employer who has provided health insurance coverage to you while employed, you have the option of continuing the health coverage for a period of time, up to two years. This continuation of coverage is called COBRA, named for the law that put it into place (Consolidated Omnibus Budget Reconciliation Act). You have to file in a timely manner for Medicare – COBRA coverage doesn’t remove that requirement.
One of the rules about Medicare Part B is that you are not required to obtain this coverage at age 65 if you’re employed and covered by a qualified health plan. Since the COBRA coverage would have been a qualified health plan if you were still employed, folks get confused about this and believe that they don’t need to file for Medicare Part B since they have COBRA coverage. Unfortunately, COBRA coverage doesn’t meet the requirements – if you have COBRA, you’re not employed by that employer any longer.
This can be an onerous penalty – a 10% increase in your Part B premium per 12 months delay, for life. For 2014 this could range from an extra $125.88 up to $402.84 per year in increased Part B premiums. The 10% increase is for each full 12 months of delay – if less than 12 months have passed since you were first eligible to enroll in Part B, no penalty applies. If, for example, you delayed enrolling for Medicare Part B for a total of 30 months, your premium would be increased by 20% (2 full 12-month periods of delay) for the rest of your life.



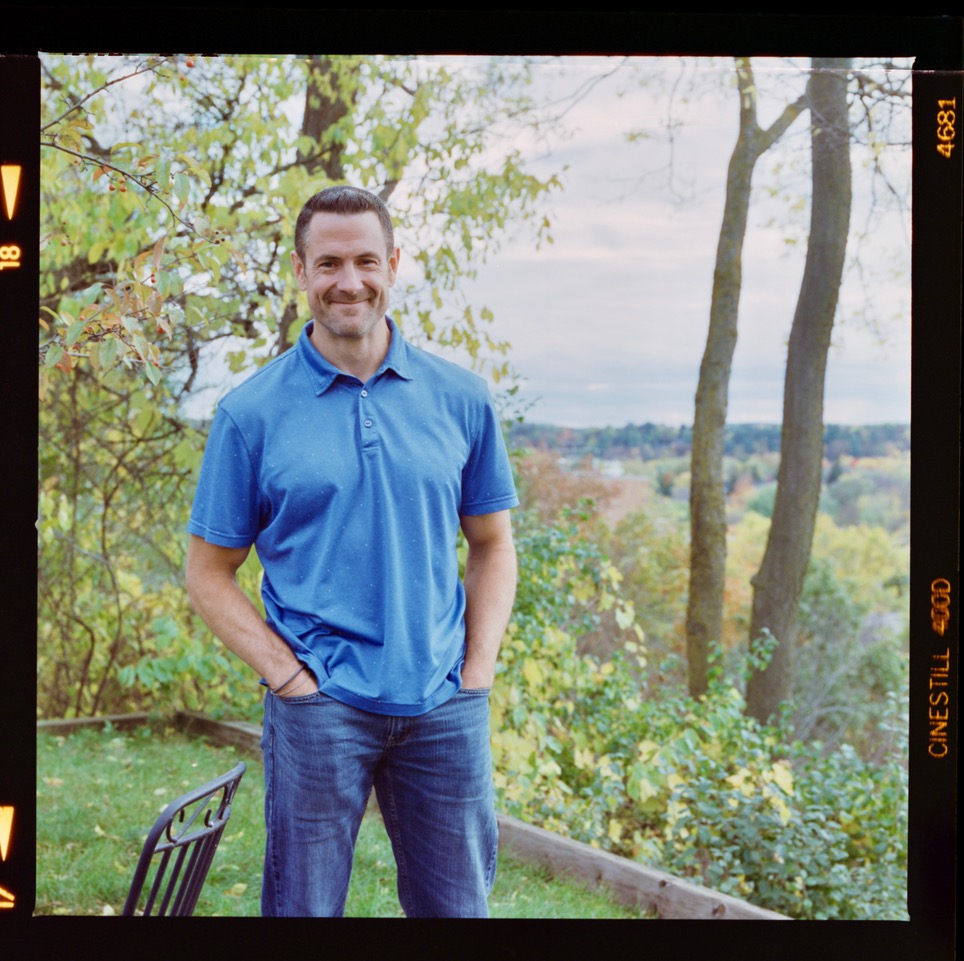 Sterling Raskie, MSFS, CFP®, ChFC®
Sterling Raskie, MSFS, CFP®, ChFC® The latest in our Owner’s Manual series, A 401(k) Owner’s Manual, was published in January 2020 and is available on
The latest in our Owner’s Manual series, A 401(k) Owner’s Manual, was published in January 2020 and is available on  A Medicare Owner’s Manual, is updated with 2020 facts and figures. This manual is available on
A Medicare Owner’s Manual, is updated with 2020 facts and figures. This manual is available on  Social Security for the Suddenly Single can be found on Amazon at
Social Security for the Suddenly Single can be found on Amazon at  Sterling’s first book, Lose Weight Save Money, can be
Sterling’s first book, Lose Weight Save Money, can be  An IRA Owner’s Manual, 2nd Edition is available for purchase on Amazon. Click the link to choose the
An IRA Owner’s Manual, 2nd Edition is available for purchase on Amazon. Click the link to choose the  Jim’s book – A Social Security Owner’s Manual, is now available on Amazon. Click this link for the
Jim’s book – A Social Security Owner’s Manual, is now available on Amazon. Click this link for the  And if you’ve come here to learn about queuing waterfowl, I apologize for the confusion. You may want to discuss your question with Lester, my loyal watchduck and self-proclaimed “advisor’s advisor”.
And if you’ve come here to learn about queuing waterfowl, I apologize for the confusion. You may want to discuss your question with Lester, my loyal watchduck and self-proclaimed “advisor’s advisor”.
One of the rules about Medicare Part B is that you are not required to obtain this coverage at age 65 if you’re employed and covered by a qualified health plan.
With regard to this statement in your article, I assume that the spouse of an employee covered by a qualified health plan, who has spousal coverage, is also exempted from having to file for Part B within three months of turning 65. Is this correct?
Thanks, Lacy Reaves
Yes, that’s correct – but to be certain you will want to check with the HR function of the employer, as well as with Medicare. It never hurts to verify.
Is Retiree coverage provided by your former employer treated the same way as Cobra? If you retired at 60 and as a retiree were provided and purchased the same group coverage that your employer used to pay for, at 65 could you opt to continue buying that coverage until Medicare is a better option for you without paying the Part B penalty?
Some retiree coverage provides an exemption as well. Your employer would have the details on that.